This article is the first of a series of posts dedicated to uterine pathologies. Here, we will explain the types of pathologies, and we will focus on uterine malformations, their causes and the different methods of diagnosis we use at Equipo Juana Crespo. Let’s start!
We call uterine pathologies to all those anomalies or diseases that affect the state and proper functioning of the uterus.
Mainly, we will differentiate two types:
- Acquired uterine pathologies
Those that develop throughout a woman’s life such as fibroids, polyps or adhesions, for example.
- Hereditary or congenital uterine pathologies
All those anomalies that we are born with. These are malformations which, both morphologically and functionally, result in a uterus of a different composition and structure compared to how it is considered anatomically normal.
But what is a normal uterus?
Morphology of the uterus
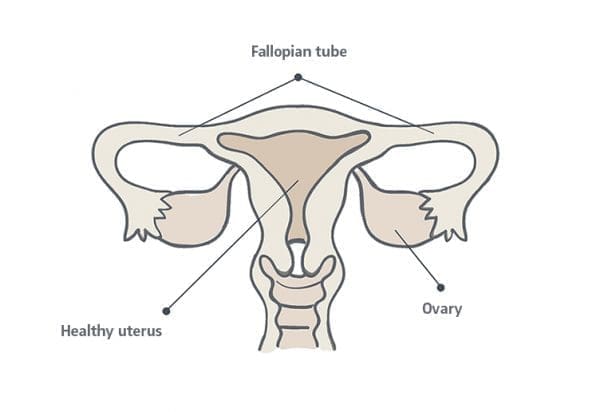
The uterus, like any part of the human body, is different in every woman. But generally, the standard uterus of an adult woman is approximately 6 to 8 centimeters long and about 5 centimeters wide.
Its shape is similar to that of an inverted triangle and an endometrium that, in fertile age -from the first period until menopause-, will not exceed 16 mm in thickness.
In this respect, it is important to distinguish between women who have or have not had previous pregnancies, as these may have been responsible for an irreversible distension of the cavity. For example, in a woman who has been pregnant several times, the length of the uterus after its recovery will surely be closer to 10 centimeters in height and 7 centimeters in width.
Uterine or Mullerian malformations
In gynecology and reproductive medicine, uterine malformations are often referred to as Müllerian malformations. As we explained, these are congenital anomalies and their name derives from the alterations in the development of the Müllerian ducts.
This part of the anatomy appears in both sexes during the embryogenesis process (phase of human development that takes place during the first eight weeks of gestation).
In the case of women, the Müllerian tubes will originate the uterine tubes and the utero-vaginal canal (formed by the uterus, the cervix and the upper part of the vagina) and it is then, when the first complications leading to future uterine malformations may arise.
Causes and consequences of a uterine malformation
When it comes to uterine malformations, it is very difficult to specify the exact figures since there are also less serious anomalies that do not produce infertility, and may even never be detected. This is because the malformations are mild and do not trigger associated symptoms. Therefore, not every uterine malformation will lead to a total or partial loss of fertility.
On the other hand, it is also true that, in the world of reproductive medicine, uterine malformations are not an isolated or rare problem. Nowadays, pathological uteruses are responsible for between 20% to 25% of all cases of infertility.
However, as we said before, only in isolated cases (and always before pregnancy) will the malformation be accompanied by symptoms such as: dysmenorrhea, irregular periods or even a total lack of bleeding.
In most cases, it is when a woman tries to become pregnant that some kind of problem becomes apparent and, consequently, she begins to seek the causes of these symptoms. Symptoms that can be:
- Implantation failures
- Ectopic pregnancies
- Repeat abortions
- Fetal malpositions
- Premature births
- Dysdynamics, etc. etc.
As a result of these problems, our fertility specialists will perform the necessary tests that will lead us to create a proper diagnosis.
Methods to diagnose uterine malformations
The diagnosis of a uterine malformation can be made through various tests, depending on the pathology and the specific location of the problem. In most cases, a transvaginal ultrasound can be sufficient, either in 2D or 3D.

In other cases, however, tests such as MRI, hysteroscopy or diagnostic laparoscopy may be necessary. Nevertheless, the tests that are most commonly used for the study of a possible uterine malformation are: firstly, magnetic resonance and, secondly, hysterosalpingography or HSG.
This last diagnostic technique is an X-ray test that makes it possible to check the condition of the fallopian tubes and the uterine cavity without the need for diagnostic surgery.
The moment of its execution must coincide with the end of menstruation (mid-follicular phase, prior to ovulation). In other words, when the upper layers of the endometrium have been expelled and the uterine cavity is in optimum condition for evaluation.